Case Study: Process Complexities Causes Frustration Among Providers & Claimants
As the healthcare industry grapples with increasingly complex claims and billing processes, the demand for timely, accurate, and transparent service has never been greater. This case study explores how DATAMARK’s innovative solutions—spanning cloud workflow automation, generative AI-powered knowledge management, and branded communication tools—empower health insurance providers to simplify operations, improve provider and member interactions, and elevate overall satisfaction. By addressing these critical challenges, DATAMARK helps healthcare organizations deliver a seamless experience that fosters trust and efficiency.

Background: Prolonged response times contribute to increased frustration among members and providers.
A leading health insurance provider faced significant challenges due to the complexity of their claims and billing processes. The intricate nature of
healthcare billing, combined with inconsistent and inefficient provider communication, led to mounting frustration among both members and healthcare providers. This complexity directly resulted in an overall decrease in customer satisfaction levels.
What are Claims and Billing Processes in Healthcare?
Claims and billing processes involve the submission, processing, and payment of insurance claims for healthcare services rendered. These processes require accurate data entry, verification of coverage, adherence to regulatory requirements, and timely communication between insurers, providers, and members. Errors or delays can lead to financial discrepancies, disputes, and strained relationships, making efficiency and transparency crucial.
Challenge: Surging Inquiries and Inefficient Support / Resolution
The complexity in claims and billing led to a surge in both inbound and outbound communications as members and providers sought clarification on billing issues, coverage details, and network information. The insurance provider’s existing support infrastructure struggled to handle the increased volume, resulting in:
- Longer Wait Times: Overloaded call centers led to extended hold times, frustrating customers seeking timely assistance.
- Inconsistent Information: Agents lacked immediate access to up-to-date information, leading to inconsistent responses.
- Decreased Satisfaction: The overall customer experience suffered, impacting reputation and member retention.
DATAMARK Solution: Cloud Workflow Automation; Generative AI Knowledge Base Implementation and Logo Branded Caller ID Delivery
DATAMARK conducted a thorough analysis of the leading healthcare insurance provider’s operational challenges and identified key areas for improvement. The tailored solution encompassed:
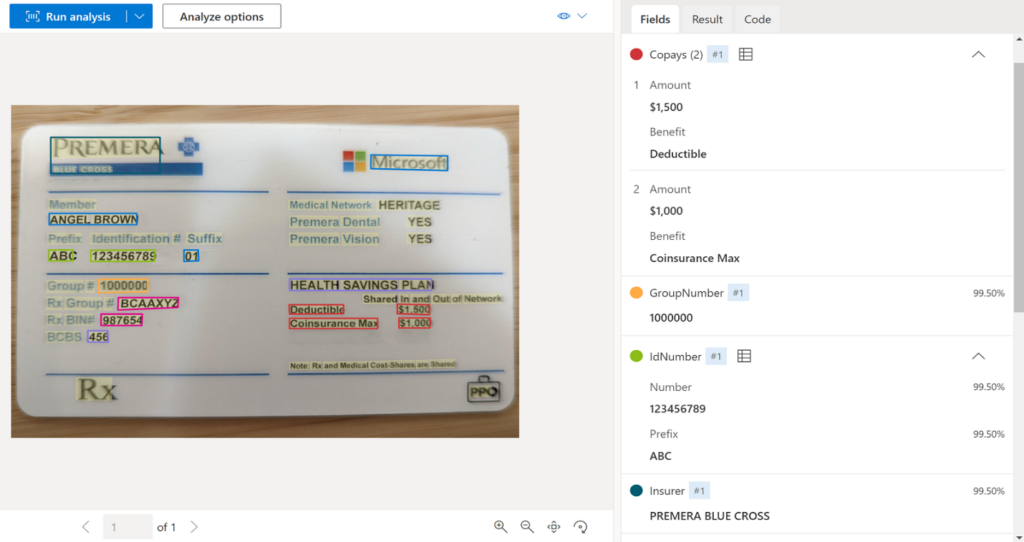
Cloud Workflow Solution: DATAMARK transitioned manual data entry and document categorization to a cloud-based automated system, streamlining the claims and billing processes. This reduced errors, accelerated processing times, and provided greater transparency. An example of OCR on a health insurance card is depicted on the right.
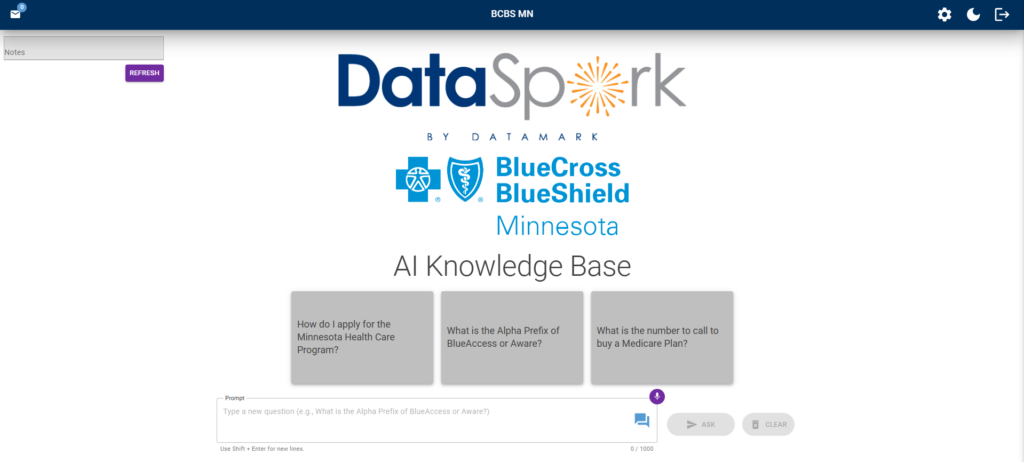
Generative AI: Knowledge Base (DataSpark) Implementation: DATAMARK introduced DataSpark, a proprietary Generative AI Knowledge Base tool designed to simplify complex questions and scenarios related to claims, coverage, and billing. This tool equipped agents with quick access to accurate, real-time information. To the left is an example of DataSpark utilizing Generative AI to answer an agent question.
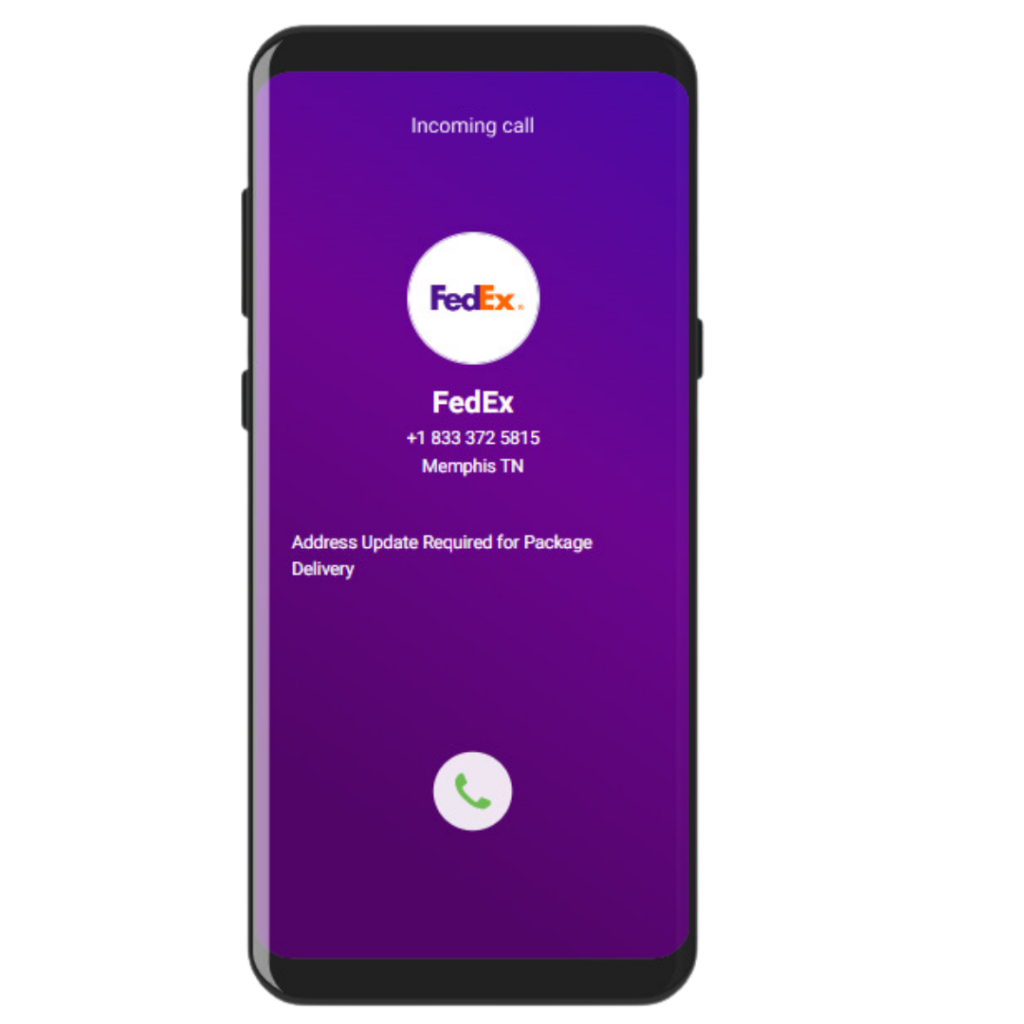
Logo Enhanced Branded Caller ID Delivery: DATAMARK is equipped with technology such as Logo Enhanced Branded Caller ID Delivery to improve outbound communication effectiveness, ensuring members recognized and trusted incoming calls from agents.
Results: Operational Efficiency and Enhanced Customer Satisfaction
The implementation of DATAMARK’s solutions yielded significant improvements in the insurance provider’s operations and customer experience:
- Reduced Claims Processing Time: The cloud workflow automation led to an overall reduction in claims and billing processing times. This acceleration minimized delays, reduced financial discrepancies, and improved cash flow for both providers and members.
- Improved Agent Efficiency and Consistency: With immediate access to accurate information through DataSpark, agents reduced their total AHT and saw an increase in their quality level objectives.
- Increased Customer Trust and Communication Effectiveness: The Logo Enhanced Branded Caller ID delivery resulted in a 37% increase in answered outbound calls. Members were more willing to engage in communications, leading to quicker resolutions and stronger relationships.
Conclusion
DATAMARK’s strategic integration of cloud workflow automation advanced AI-driven knowledge management with DataSpark, and enhanced communication tools significantly transformed the insurance provider’s operations. By streamlining complex claims and billing processes, empowering customer service agents with real-time information, and fostering trust through branded communications, DATAMARK addressed the core challenges affecting customer satisfaction.
Interested to learn more, contact us at datamark.net!
WANT TO KEEP READING?
MORE DATAMARK CASE STUDIES
We help Fortune 500 companies, large enterprises and government agencies address the greatest challenges to their businesses to increase their profitability as they grow. Explore the case studies below to learn how we’ve helped our customers and how we can help your business, as well.





